Health
What is the UK Covid inquiry and how does it work?
A probe examining the government’s response to the pandemic has gathered testimony from a range of individuals, including politicians, civil servants, specialists, and families who have lost loved ones.
The Covid-19 Inquiry has commenced its examination of the measures implemented to support workers' incomes and maintain business operations during the pandemic.

This development follows the release of the inquiry's second report, which criticized the government's Covid response as inadequate and untimely.
Between March 2020 and May 2023, when the World Health Organization declared the end of the "global health emergency", approximately 227,000 individuals in the UK lost their lives to Covid.
In June 2022, former UK Prime Minister Boris Johnson initiated the Covid-19 Inquiry, more than a year after announcing that the government's pandemic response would undergo scrutiny.
The launch of the inquiry came after the Covid-19 Bereaved Families for Justice campaign group threatened a judicial review, citing concerns about delays.
The inquiry's scope encompasses decision-making by the UK government, as well as the administrations in Scotland, Wales, and Northern Ireland, with the first public hearings taking place in June 2023.
Public inquiries, established and funded by the government, are led by an independent chair and possess the authority to compel witnesses to provide testimony.

These inquiries do not result in findings of guilt or innocence but instead publish conclusions and recommendations, which the government is not obligated to accept.
The chair of the Covid inquiry is Baroness Hallett, a former judge and crossbench peer who previously led the inquests into the 7 July London bombings.
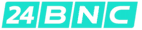
As of December 2025, the BBC has learned that the inquiry's costs have exceeded £100m, according to government figures.
This amount is in addition to the £192m spent by the inquiry itself, resulting in a total cost to taxpayers that is over 50% higher than previously estimated.
The inquiry's third stage will examine the unprecedented economic measures implemented during the first lockdown in March 2020.
The government allocated over £140bn to support businesses, with a significant portion used to fund wages for individuals forced to stay at home, including 11.7 million jobs covered by the furlough scheme between March 2020 and September 2021.
Other support measures included schemes for self-employed individuals, business loans, and business rates relief.
However, questions have been raised regarding the scope of financial support and the effectiveness of safeguards against fraud and errors.
This stage of the inquiry, scheduled to conclude before Christmas, has received over 8,000 submissions from the public, including accounts from business owners who were forced to lay off staff or close their operations, as well as employees who feared for their job security.
Former Prime Minister Rishi Sunak, who served as chancellor during the pandemic, is expected to provide further testimony about his role during these hearings.
The inquiry's second report examined political decision-making and suggested that lockdown measures might have been avoided if voluntary steps, such as social distancing and isolation, had been implemented earlier than 16 March 2020.
According to the report, a one-week delay resulted in approximately 23,000 additional deaths in England during the first wave of the pandemic.
The report also described a "toxic and chaotic" culture within the UK government during its pandemic response, which allegedly impacted the quality of advice and decision-making.
Over 7,000 documents from the time, including WhatsApp chats, emails, private diaries, and confidential files, have been made public.
The first report, focusing on resilience and preparedness, was published in July 2024.
In the report, Baroness Hallett stated that the UK was "ill-prepared" to handle a catastrophic emergency like the coronavirus pandemic.
She emphasized that the country must learn from its mistakes to prevent similar tragedies in the future, saying, "Never again can a disease be allowed to lead to so many deaths and so much suffering."
The 217-page report argued that the UK had planned for the wrong type of pandemic, leading to the untested policy of lockdown.
The report concluded that the UK government and devolved nations "failed their citizens" and that ministers did not adequately challenge scientific experts.
It provided recommendations for reforming the government's approach to emergency planning.
The inquiry is ongoing, with investigations into other aspects of the pandemic still underway.
The final public hearings are scheduled to begin in February 2026.
The inquiry will publish multiple reports, including the conclusions of each module.
A separate inquiry into the pandemic is being conducted in Scotland.
The inquiry has heard testimony from hundreds of witnesses, including current and former politicians, civil servants, government advisers, public health experts, and representatives of bereaved families.
Many witnesses have been critical of former Prime Minister Boris Johnson, who led the country throughout the pandemic.
During his first evidence session in December 2023, Johnson apologized for the "pain, loss, and suffering" caused by the pandemic.
Johnson acknowledged that mistakes were made and that "there were unquestionably things we should have done differently", but maintained that ministers had done their best in challenging circumstances.
Former Chancellor Rishi Sunak also apologized for the suffering caused by the government's actions during his first appearance before the inquiry.
However, Sunak denied that his Eat Out to Help Out Scheme had contributed to increased infections and deaths.
The government's chief medical officer, Prof Sir Chris Whitty, and former chief scientific adviser Sir Patrick Vallance, had previously told the inquiry that they were not consulted about the policy.

Sir Patrick, Sir Chris, and his former deputy Prof Sir Jonathan Van-Tam also reported receiving substantial abuse from the public while performing their duties.
Former Health Secretary Matt Hancock has provided evidence to the inquiry on multiple occasions.

During his testimony, he expressed that the UK's approach to the pandemic was flawed from the start, acknowledging that a lockdown should have been implemented earlier.
Hancock also addressed the allegedly "toxic culture" within the government, placing blame on Dominic Cummings, a former adviser to Johnson.
In his testimony, Cummings portrayed a government in disarray, sharply criticizing Johnson's handling of the situation.
The inquiry examined a series of text messages sent by Cummings, which included derogatory remarks about various ministers and officials.
Cummings expressed regret over the controversy surrounding his visit to Barnard Castle during the initial lockdown but maintained that it did not erode public confidence in the government.
The inquiry has also received testimony from leaders of the Scottish, Welsh, and Northern Irish governments, among others.
Organizations representing families who have lost loved ones are pushing for the inquiry to amplify their stories and concerns.
By the time the inquiry's submission period closed in May 2025, the Every Story Matters project had collected over 47,000 personal Covid-19 accounts.
The public can apply to attend inquiry hearings in person, allowing them to observe the proceedings directly.
For those unable to attend, the inquiry streams its public hearings on its official YouTube channel.
Furthermore, transcripts of witness testimonies are made available on the inquiry's website for public access.
Health
Study Explores if Brain Stimulation Can Reduce Selfish Behavior
Researchers have found a way to temporarily and marginally decrease self-centered behavior in individuals by activating two specific regions of the brain.
Researchers have made a groundbreaking discovery, finding that temporary reductions in selfish behavior can be achieved by stimulating specific areas of the brain.
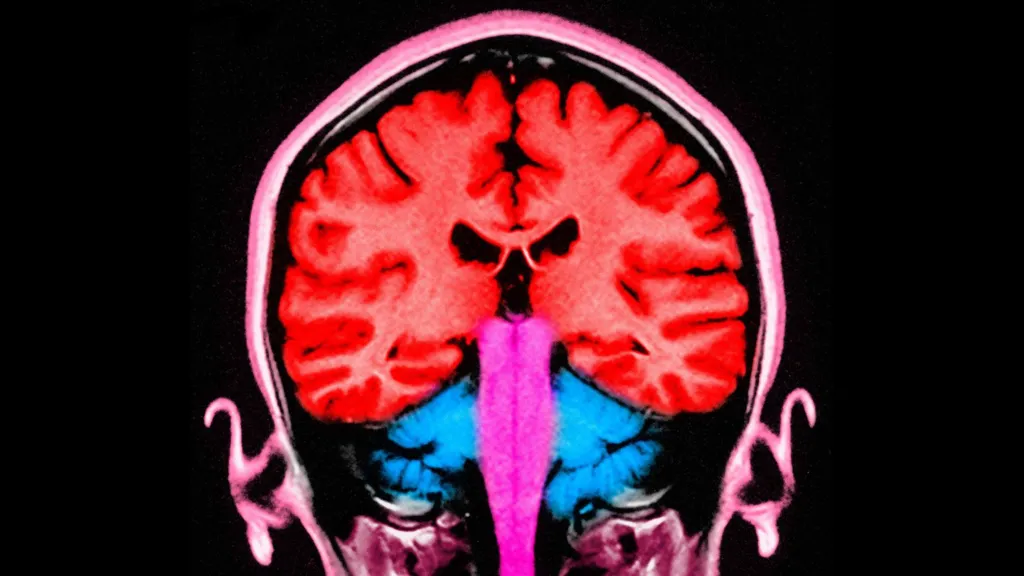
A recent study conducted at the University of Zurich involved 44 participants who were tasked with dividing a sum of money between themselves and an anonymous partner, allowing scientists to observe their decision-making processes.
The experiment utilized electrical current to stimulate the frontal and parietal regions of the brain, located at the front and rear of the skull, respectively. When these areas were stimulated simultaneously, participants exhibited a greater willingness to share their funds.
According to Prof Christian Ruff, a lead author of the study, the observed effects were consistent, albeit modest in scale.
Statistical analysis revealed a notable increase in participants' willingness to allocate funds to others, indicating a shift in their behavior.
The findings not only provide insight into the neural mechanisms underlying fundamental human behavior but may also have implications for the treatment of certain brain disorders characterized by impaired social behavior.
Prof Ruff noted that some individuals struggle with profound social difficulties due to an inability to consider others' perspectives, leading to consistently selfish behavior, and suggested that this discovery could potentially be used to address such issues.
However, the effects of the brain stimulation were found to be short-lived, suggesting that repeated application may be necessary to achieve lasting changes.
Prof Ruff likened the potential effects of repeated stimulation to the benefits of regular exercise, stating that consistent application over a prolonged period could lead to significant changes in behavior, much like the physical adaptations that occur with regular gym attendance.
This latest discovery builds upon a previous study in which researchers monitored brain activity while participants engaged in a similar money-sharing game, providing a foundation for the current findings.
The earlier study identified two brain regions that appeared to be synchronized, with neural activity occurring at the same frequency, when participants made more generous decisions.
These brain areas are known to play a crucial role in decision-making and empathy, enabling individuals to distinguish between their own feelings and those of others.
When participants made selfless decisions, the regions responsible for empathy and decision-making were found to be communicating with each other.
The researchers sought to investigate whether electrical stimulation could be used to influence this communication and promote more selfless decision-making.
One participant who underwent the brain stimulation test described the experience as a gentle, soothing sensation, comparable to a warm shower or light rain on the scalp.
The participant reported making decisions while receiving the stimulation without feeling any external influence on their choices.
The discovery of a consistent neural pattern associated with selfless decision-making across multiple individuals suggests that altruism may be an innate, evolutionarily conserved trait that enables humans to care for one another.
Prof Ruff emphasized the clinical significance of this finding, highlighting the potential to modify and influence this neural mechanism.
Dr Jie Hu, a co-author of the study, noted that the research provides evidence of a causal relationship between brain activity and decision-making, demonstrating that targeted stimulation can alter an individual's sharing behavior.
By manipulating communication within a specific brain network using non-invasive stimulation, the researchers observed a shift in participants' decisions, influencing the balance between self-interest and altruism.
Addressing concerns about the potential implications of this research, Prof Ruff assured that the experiment was conducted with strict adherence to medical regulations and ethical guidelines, ensuring the well-being and informed consent of all participants.
The neuroscientist drew a distinction between the controlled, medically regulated nature of the experiment and the often-subliminal influences of social media and advertising, which can affect behavior without explicit consent.
Prof Ruff suggested that, in contrast to the experiment, the impacts of social media and advertising on brain function and behavior are often unforeseen and uncontrolled, highlighting the importance of careful consideration and regulation in such contexts.
Health
NHS Workers to Receive 3.3% Pay Increase
Labor unions have expressed displeasure, yet the government maintains that its actions showcase a dedication to its workforce.
The government has confirmed that NHS staff in England will receive a 3.3% pay increase in the upcoming financial year.

This pay award applies to approximately 1.4 million health workers, including nurses, midwives, physiotherapists, and porters, but excludes doctors, dentists, and senior management.
Although the Department of Health and Social Care initially proposed a lower figure, it has accepted the recommendation of the independent pay review body to demonstrate its commitment to NHS staff, resulting in a higher pay rise than initially suggested.
However, several health unions have expressed disappointment with the announced pay award.
Prof Nicola Ranger, general secretary of the Royal College of Nursing (RCN), noted that the 3.3% increase falls short of the current consumer price index (CPI) inflation rate of 3.4%, which measures the rise in prices over the past year.
Prof Ranger stated, "A pay award that is lower than the current inflation rate is unacceptable, and unless inflation decreases, the government will be imposing a real pay cut on NHS workers."
She criticized the government's approach, saying, "This strategy of making last-minute decisions is not an appropriate way to treat individuals who are essential to a system in crisis."
Prof Ranger indicated that she would wait to see the pay awards for the rest of the public sector and doctors before deciding on a course of action.
The RCN had previously reacted strongly to the 5.4% pay increase received by resident doctors last year, compared to the 3.6% increase received by nurses, which they described as "grotesque".
Prof Ranger emphasized, "Nursing staff will not accept being treated with disrespect, as has happened in the past when they were given lower pay awards than other groups."
Helga Pile, head of health at Unison, the largest health union, commented, "NHS staff who are already under financial pressure will be outraged by another pay award that fails to keep up with inflation."
"Once again, they are expected to deliver more while their pay effectively decreases, as it falls behind the rising cost of living," she added.
In response, the government argued that the pay award is actually above the forecasted inflation rate for the coming year, which is around 2%.
A spokesperson for the Department of Health and Social Care stated, "This government greatly values the outstanding work of NHS staff and is committed to supporting them."
The pay increase is expected to be implemented by the start of April.
However, the government did not provide a timeline for the announcement on doctors' pay, as the pay review body responsible for making recommendations on their pay has yet to submit its report to ministers.
The government is currently engaged in negotiations with the British Medical Association regarding the pay of resident doctors, previously known as junior doctors.
Members of the BMA recently voted in favor of strike action, granting them a six-month mandate for walkouts, and there have been 14 strikes so far in the ongoing dispute.
Health
NHS Waiting List Hits Three-Year Low
In England, the backlog has fallen below 7.3 million for the first time since 2023, yet worries persist regarding prolonged waiting times in accident and emergency departments.
England's hospital waiting list has reached its lowest point in almost three years, marking a significant milestone in the country's healthcare system.

As of December 2025, the number of patients awaiting treatment, including knee and hip operations, stood at 7.29 million, the lowest figure recorded since February 2023.
However, the latest monthly update from NHS England reveals that long wait times persist in Accident and Emergency departments, with a record number of patients experiencing 12-hour trolley waits.
In January 2026, over 71,500 patients spent more than 12 hours waiting for a hospital bed after being assessed by A&E staff, the highest number tracked since 2010.
This translates to nearly one in five patients admitted after visiting A&E waiting for an extended period.
According to Health Secretary Wes Streeting, while progress has been made, significant challenges still need to be addressed.
Streeting acknowledged that "there is much more to do" and emphasized the need to accelerate progress, but expressed optimism that the NHS is on the path to recovery.
Dr. Vicky Price, representing the Society for Acute Medicine, noted that hospitals are operating beyond safe capacity in terms of emergency care.
Dr. Price highlighted the vulnerability of patients who require admission, often elderly and frail individuals with complex needs, who are at greater risk of harm when care is delivered in corridors and hospitals exceed safe limits.
Duncan Burton, Chief Nursing Officer for England, commended the progress made in reducing wait times, achieved despite the challenges posed by strikes by resident doctors.
Burton attributed this progress to the hard work and dedication of NHS staff, describing it as a "triumph".
Although the waiting list decreased, performance against the 18-week target slightly declined, with 61.5% of patients waiting less than 18 weeks, compared to 61.8% in November, and still short of the 92% target set to be met by 2029.
Rory Deighton of the NHS Confederation, which represents hospitals, welcomed the progress but cautioned that it obscures significant regional variations.
A recent BBC report revealed that nearly a quarter of hospital trusts experienced worsening wait times over the past year.
Deighton emphasized that the NHS is composed of numerous separate organizations, each with unique financial and operational challenges, making it more difficult to address care backlogs in some areas.
According to Deighton, this means that tackling care backlogs will be more challenging in certain parts of the country due to these distinct regional challenges.
-

 News9 hours ago
News9 hours agoAustralian Politics Faces Questions Over Gender Equality Amid Sussan Ley’s Appointment
-
 News7 hours ago
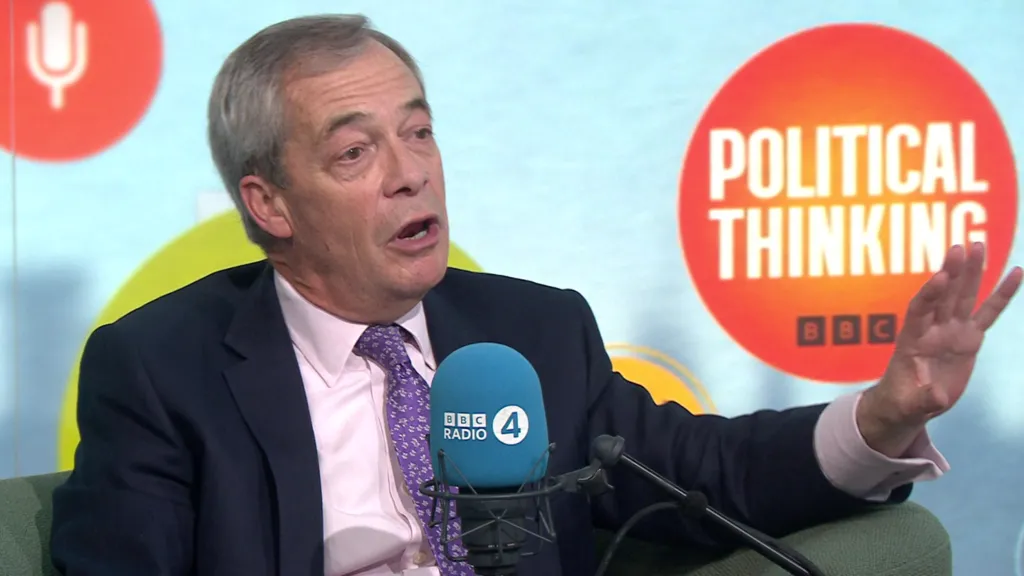
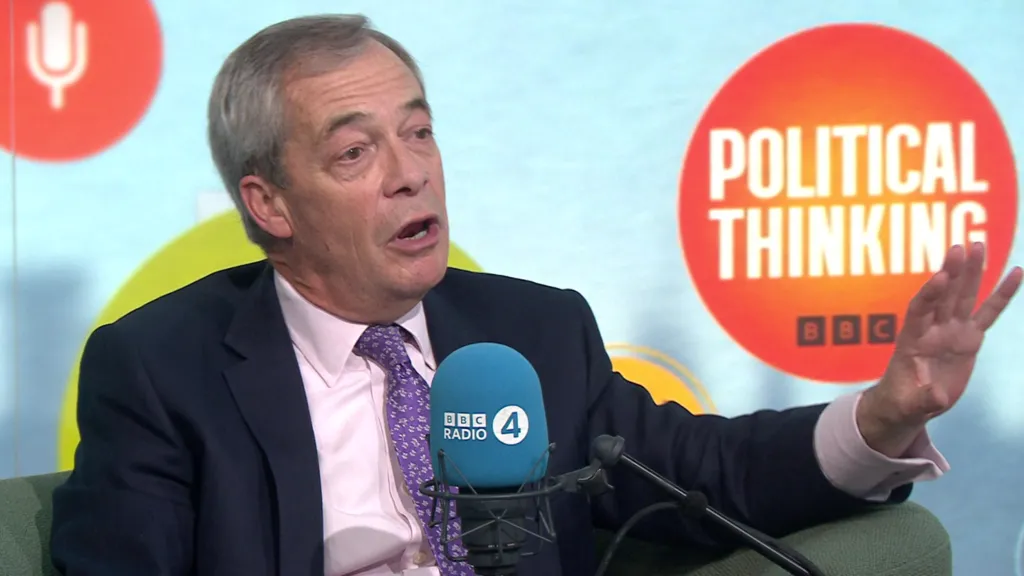
News7 hours agoFarage Says Reform to Replace Traditional Tory Party
-

 News7 hours ago
News7 hours agoWrexham Pair Seek Win Against Former Team Ipswich
-

 News12 hours ago
News12 hours agoLiberal Party Removes Australia’s First Female Leader
-

 News10 hours ago
News10 hours agoUK Braces for Cold Snap with Snow and Ice Alerts Expected
-
 News7 hours ago
News7 hours agoHusband’s alleged £600k theft for sex and antiques blamed on drug side effects
-

 News2 days ago
News2 days agoSunbed ads spreading harmful misinformation to young people
-

 Business12 hours ago
Business12 hours agoBBC Reporter Exposed to Cyber Attack Due to Vulnerabilities in AI Coding Tool