Health
GP-provided financial assistance improves patient health outcomes
A new initiative in London is exploring the connection between financial concerns and well-being, with local GPs testing a pilot program aimed at providing financial assistance.
A unique initiative in south London is providing financial guidance to patients at GP surgeries, helping them manage debt and navigate benefits claims, with notable outcomes.

The Back on Track scheme, operating in 34 practices across Lambeth and Southwark, has resulted in one-third of patients reducing their GP visits, while over 1,100 individuals have successfully secured benefits, resolved debts, or experienced decreased stress levels.
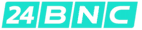
A 62-year-old Stockwell resident, Ife, has benefited from the program, which she discovered through her local GP surgery.
Ife suffers from chronic arthritis pain and had accumulated energy debt after being forced to quit her job due to mobility issues while awaiting knee replacement surgery.
Despite her limited mobility, Ife's Capability Benefit claim was denied, exacerbating her financial concerns and negatively impacting her mental well-being.
However, with the assistance of a financial support link worker from the Back on Track program, Ife successfully appealed the Universal Credit decision and secured disability benefits, in addition to receiving help with her energy and water debts through an affordable payment plan.
Ife expressed her gratitude, stating that the program was a relief, and the support she received helped her manage the complex claims process for Personal Independence Payment and Universal Credit.
She added that she is now referring friends in similar situations and has significantly reduced her GP visits, citing a notable improvement in her overall well-being.
The Financial Shield project, led by Impact on Urban Health, aims to alleviate financial stress and demonstrate its impact on patients' health, ultimately freeing up GPs to focus on medical care.

According to Impact on Urban Health, more than half of the participants have reported improvements in their health after receiving targeted support, including assistance with securing benefits, debt write-offs, and creditor negotiations.
Vikesh Sharma, a south London GP participating in the scheme, shared the story of a woman in her 40s who visited the surgery several times for heart palpitations, which were later linked to severe stress caused by rent worries and debt.
Dr. Sharma noted that being able to identify the root cause of the patient's symptoms and offer immediate support transformed the consultation, enabling him to address the patient's financial health as a central aspect of her care.
He emphasized the importance of providing a solution to the patient's financial concerns, rather than simply acknowledging them, in order to effectively address the underlying issues.
The patient returned six months later, reflecting on how stress had affected her health and taking steps to improve it, demonstrating the positive impact of the program.
Michael Parsons, head of the Financial Foundations Programme at Impact on Urban Health, explained to BBC London that financial difficulties often exacerbate health problems, creating a cycle that requires targeted intervention to break.
Parsons noted that people with poor health are more likely to experience financial troubles, highlighting the need for initiatives that address both aspects.
He added that the majority of participants in the scheme report improved mental and physical health, demonstrating the program's effectiveness.
Furthermore, the scheme has led to a reduction in GP visits, indicating a link between financial stability and improved health outcomes.
The Financial Shield aims to embed financial support within GP surgeries, allowing doctors to focus on medical treatment while patients address the root causes of stress, resulting in a more efficient and preventative approach to healthcare.
The NHS stated that decisions regarding the service would be made locally, and the impact of the program would be assessed within the Lambeth and Southwark systems, with each integrated care board responsible for determining potential wider rollout.
The government's 10 Year Health Plan includes plans to integrate debt support into new neighborhood health services, aligning with the goals of the Financial Shield model.
Impact on Urban Health noted that the Financial Shield builds upon the London Health Board's objective of providing welfare advice to all Londoners in need.
Health
Study Explores if Brain Stimulation Can Reduce Selfish Behavior
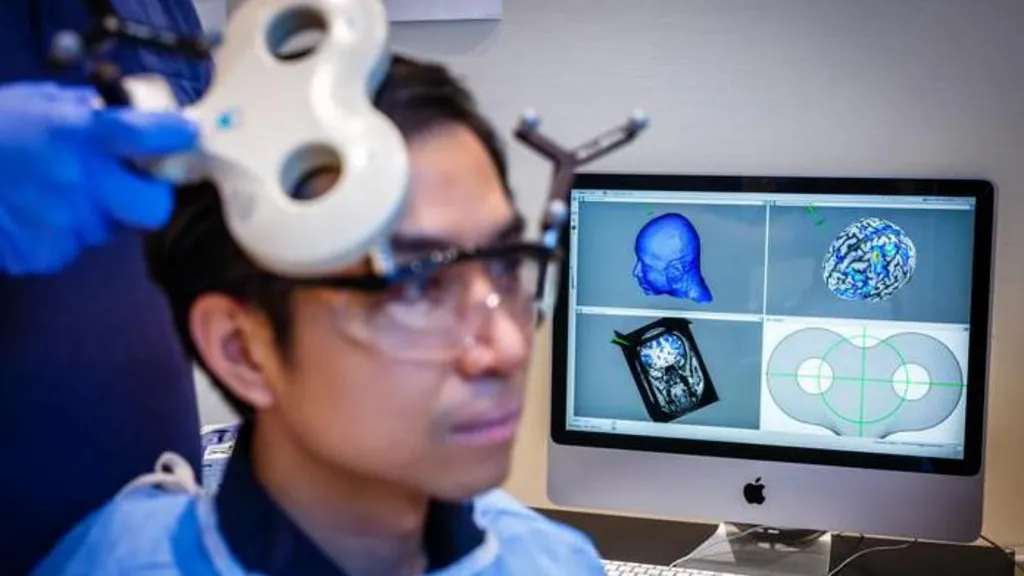
Researchers have found a way to temporarily and marginally decrease self-centered behavior in individuals by activating two specific regions of the brain.
Researchers have made a groundbreaking discovery, finding that temporary reductions in selfish behavior can be achieved by stimulating specific areas of the brain.
A recent study conducted at the University of Zurich involved 44 participants who were tasked with dividing a sum of money between themselves and an anonymous partner, allowing scientists to observe their decision-making processes.
The experiment utilized electrical current to stimulate the frontal and parietal regions of the brain, located at the front and rear of the skull, respectively. When these areas were stimulated simultaneously, participants exhibited a greater willingness to share their funds.
According to Prof Christian Ruff, a lead author of the study, the observed effects were consistent, albeit modest in scale.
Statistical analysis revealed a notable increase in participants' willingness to allocate funds to others, indicating a shift in their behavior.
The findings not only provide insight into the neural mechanisms underlying fundamental human behavior but may also have implications for the treatment of certain brain disorders characterized by impaired social behavior.
Prof Ruff noted that some individuals struggle with profound social difficulties due to an inability to consider others' perspectives, leading to consistently selfish behavior, and suggested that this discovery could potentially be used to address such issues.
However, the effects of the brain stimulation were found to be short-lived, suggesting that repeated application may be necessary to achieve lasting changes.
Prof Ruff likened the potential effects of repeated stimulation to the benefits of regular exercise, stating that consistent application over a prolonged period could lead to significant changes in behavior, much like the physical adaptations that occur with regular gym attendance.
This latest discovery builds upon a previous study in which researchers monitored brain activity while participants engaged in a similar money-sharing game, providing a foundation for the current findings.
The earlier study identified two brain regions that appeared to be synchronized, with neural activity occurring at the same frequency, when participants made more generous decisions.
These brain areas are known to play a crucial role in decision-making and empathy, enabling individuals to distinguish between their own feelings and those of others.
When participants made selfless decisions, the regions responsible for empathy and decision-making were found to be communicating with each other.
The researchers sought to investigate whether electrical stimulation could be used to influence this communication and promote more selfless decision-making.
One participant who underwent the brain stimulation test described the experience as a gentle, soothing sensation, comparable to a warm shower or light rain on the scalp.
The participant reported making decisions while receiving the stimulation without feeling any external influence on their choices.
The discovery of a consistent neural pattern associated with selfless decision-making across multiple individuals suggests that altruism may be an innate, evolutionarily conserved trait that enables humans to care for one another.
Prof Ruff emphasized the clinical significance of this finding, highlighting the potential to modify and influence this neural mechanism.
Dr Jie Hu, a co-author of the study, noted that the research provides evidence of a causal relationship between brain activity and decision-making, demonstrating that targeted stimulation can alter an individual's sharing behavior.
By manipulating communication within a specific brain network using non-invasive stimulation, the researchers observed a shift in participants' decisions, influencing the balance between self-interest and altruism.
Addressing concerns about the potential implications of this research, Prof Ruff assured that the experiment was conducted with strict adherence to medical regulations and ethical guidelines, ensuring the well-being and informed consent of all participants.
The neuroscientist drew a distinction between the controlled, medically regulated nature of the experiment and the often-subliminal influences of social media and advertising, which can affect behavior without explicit consent.
Prof Ruff suggested that, in contrast to the experiment, the impacts of social media and advertising on brain function and behavior are often unforeseen and uncontrolled, highlighting the importance of careful consideration and regulation in such contexts.
Health
NHS Workers to Receive 3.3% Pay Increase
Labor unions have expressed displeasure, yet the government maintains that its actions showcase a dedication to its workforce.
The government has confirmed that NHS staff in England will receive a 3.3% pay increase in the upcoming financial year.

This pay award applies to approximately 1.4 million health workers, including nurses, midwives, physiotherapists, and porters, but excludes doctors, dentists, and senior management.
Although the Department of Health and Social Care initially proposed a lower figure, it has accepted the recommendation of the independent pay review body to demonstrate its commitment to NHS staff, resulting in a higher pay rise than initially suggested.
However, several health unions have expressed disappointment with the announced pay award.
Prof Nicola Ranger, general secretary of the Royal College of Nursing (RCN), noted that the 3.3% increase falls short of the current consumer price index (CPI) inflation rate of 3.4%, which measures the rise in prices over the past year.
Prof Ranger stated, "A pay award that is lower than the current inflation rate is unacceptable, and unless inflation decreases, the government will be imposing a real pay cut on NHS workers."
She criticized the government's approach, saying, "This strategy of making last-minute decisions is not an appropriate way to treat individuals who are essential to a system in crisis."
Prof Ranger indicated that she would wait to see the pay awards for the rest of the public sector and doctors before deciding on a course of action.
The RCN had previously reacted strongly to the 5.4% pay increase received by resident doctors last year, compared to the 3.6% increase received by nurses, which they described as "grotesque".
Prof Ranger emphasized, "Nursing staff will not accept being treated with disrespect, as has happened in the past when they were given lower pay awards than other groups."
Helga Pile, head of health at Unison, the largest health union, commented, "NHS staff who are already under financial pressure will be outraged by another pay award that fails to keep up with inflation."
"Once again, they are expected to deliver more while their pay effectively decreases, as it falls behind the rising cost of living," she added.
In response, the government argued that the pay award is actually above the forecasted inflation rate for the coming year, which is around 2%.
A spokesperson for the Department of Health and Social Care stated, "This government greatly values the outstanding work of NHS staff and is committed to supporting them."
The pay increase is expected to be implemented by the start of April.
However, the government did not provide a timeline for the announcement on doctors' pay, as the pay review body responsible for making recommendations on their pay has yet to submit its report to ministers.
The government is currently engaged in negotiations with the British Medical Association regarding the pay of resident doctors, previously known as junior doctors.
Members of the BMA recently voted in favor of strike action, granting them a six-month mandate for walkouts, and there have been 14 strikes so far in the ongoing dispute.
Health
NHS Waiting List Hits Three-Year Low
In England, the backlog has fallen below 7.3 million for the first time since 2023, yet worries persist regarding prolonged waiting times in accident and emergency departments.
England's hospital waiting list has reached its lowest point in almost three years, marking a significant milestone in the country's healthcare system.

As of December 2025, the number of patients awaiting treatment, including knee and hip operations, stood at 7.29 million, the lowest figure recorded since February 2023.
However, the latest monthly update from NHS England reveals that long wait times persist in Accident and Emergency departments, with a record number of patients experiencing 12-hour trolley waits.
In January 2026, over 71,500 patients spent more than 12 hours waiting for a hospital bed after being assessed by A&E staff, the highest number tracked since 2010.
This translates to nearly one in five patients admitted after visiting A&E waiting for an extended period.
According to Health Secretary Wes Streeting, while progress has been made, significant challenges still need to be addressed.
Streeting acknowledged that "there is much more to do" and emphasized the need to accelerate progress, but expressed optimism that the NHS is on the path to recovery.
Dr. Vicky Price, representing the Society for Acute Medicine, noted that hospitals are operating beyond safe capacity in terms of emergency care.
Dr. Price highlighted the vulnerability of patients who require admission, often elderly and frail individuals with complex needs, who are at greater risk of harm when care is delivered in corridors and hospitals exceed safe limits.
Duncan Burton, Chief Nursing Officer for England, commended the progress made in reducing wait times, achieved despite the challenges posed by strikes by resident doctors.
Burton attributed this progress to the hard work and dedication of NHS staff, describing it as a "triumph".
Although the waiting list decreased, performance against the 18-week target slightly declined, with 61.5% of patients waiting less than 18 weeks, compared to 61.8% in November, and still short of the 92% target set to be met by 2029.
Rory Deighton of the NHS Confederation, which represents hospitals, welcomed the progress but cautioned that it obscures significant regional variations.
A recent BBC report revealed that nearly a quarter of hospital trusts experienced worsening wait times over the past year.
Deighton emphasized that the NHS is composed of numerous separate organizations, each with unique financial and operational challenges, making it more difficult to address care backlogs in some areas.
According to Deighton, this means that tackling care backlogs will be more challenging in certain parts of the country due to these distinct regional challenges.
-

 News8 hours ago
News8 hours agoAustralian Politics Faces Questions Over Gender Equality Amid Sussan Ley’s Appointment
-
 News5 hours ago
News5 hours agoFarage Says Reform to Replace Traditional Tory Party
-

 News5 hours ago
News5 hours agoWrexham Pair Seek Win Against Former Team Ipswich
-

 News11 hours ago
News11 hours agoLiberal Party Removes Australia’s First Female Leader
-

 News9 hours ago
News9 hours agoUK Braces for Cold Snap with Snow and Ice Alerts Expected
-
 News5 hours ago
News5 hours agoHusband’s alleged £600k theft for sex and antiques blamed on drug side effects
-

 News2 days ago
News2 days agoSunbed ads spreading harmful misinformation to young people
-

 Business11 hours ago
Business11 hours agoBBC Reporter Exposed to Cyber Attack Due to Vulnerabilities in AI Coding Tool