Health
English neighborhood’s innovative approach to NHS reform
A region is set to introduce a new approach to its healthcare services, potentially alleviating GP waiting lists and freeing up hospital beds, amidst a backdrop of low public satisfaction with the NHS, which currently stands at 21%.
This article is also available to listen to on the BBC Sounds platform.

A recent summit in London brought together ministers, health professionals, and members of the public to discuss the 10-year plan for the NHS in England, which aims to address the record-low public satisfaction of 21% and a waiting list of nearly 7.5 million patients.
A key strategy being explored is shifting healthcare from hospitals to community-based care, which research suggests could be more cost-effective, with every £100 spent on community care potentially saving £31 compared to hospital care.
Health Secretary Wes Streeting has expressed his commitment to transforming the NHS into a more community-focused service, with the goal of providing better care at a lower cost.
The Washwood Heath community health clinic in east Birmingham, established two years ago, serves as a model for this approach, bringing together hospital doctors, GPs, nurses, and other healthcare professionals under one roof to provide comprehensive care.
The clinic offers a range of services, including urgent treatment, diagnostic testing, mental health care, and social support, all aimed at addressing the complex needs of the local population.

By providing a holistic approach to care, the clinic's staff can address not only physical health issues but also social problems, such as housing and daily living challenges, to help patients recover and thrive.
The clinic's primary focus is on supporting the most frequent users of health services, with the aim of keeping them out of hospital and improving their overall well-being.
According to Richard Kirby, head of Birmingham Community Healthcare NHS Trust, the clinic's approach is centered on working with the 10% of the population that accounts for 70-80% of healthcare usage, recognizing that the NHS cannot meet these individuals' needs alone.
Health Secretary Wes Streeting has expressed his support for the Washwood Heath model, describing it as a "pioneering service" that could be replicated nationwide.
However, some experts have raised questions about the feasibility of scaling up this approach, despite its potential benefits, citing concerns about resource allocation and systemic challenges.
At the heart of the clinic is a team that uses data and technology to monitor patients' progress, identify those at risk, and coordinate care to prevent hospital admissions.
The team employs various strategies, including remote monitoring and equipment provision, to support patients in their homes and reduce the need for hospitalization.
The clinic's staff are alerted in real-time when a patient requires emergency care, allowing for swift intervention and coordination with hospital teams to facilitate discharge and ongoing support.

Nurse Dani Fullerton notes that her role at the clinic is distinct from her previous experiences, as she works to identify patients who would benefit from the clinic's services and develop personalized care plans.
The clinic's staff have identified loneliness as a key factor in hospital admissions and are working to address this issue through targeted support and community engagement.
Research has shown that severe loneliness can have significant costs, exceeding £9,500 per person, due to its impact on well-being, health, and productivity.
To combat loneliness, the clinic's staff collaborate with local charities and council services to provide comprehensive support, including social activities and practical assistance.
Social prescriber Christine Francis works with patients to connect them with community groups and services, recognizing that loneliness often underlies frequent hospital visits.
By linking patients with befriending services, social activities, and other forms of support, Ms. Francis aims to help individuals build connections and reduce their reliance on healthcare services.
The clinic's staff also address related issues, such as hoarding and house cleaning, to promote overall well-being and mental health.
While some experts have raised questions about the evidence base for social prescribing, the clinic's staff are convinced of its effectiveness, citing firsthand observations of positive outcomes.
Occupational therapist Hamzisah Aslam recalls a visit to a patient's home, where a multidisciplinary team worked together to develop a care plan, demonstrating the benefits of collaborative working.
The team's ability to respond quickly and effectively was facilitated by their integrated approach, which allowed for rapid decision-making and action.
Local GPs have also reported positive outcomes, with one practice estimating that the clinic's support freed up over 100 appointments in six months, enabling them to offer longer consultations to patients who needed them.

Dr. Subeena Suleman notes that the clinic's intervention allowed her practice to allocate more time to other patients, resulting in improved care and increased patient satisfaction.
Since its launch, the Washwood Heath clinic has reported significant reductions in GP visits (31%), A&E attendances (20%), and hospital admissions (21%) among the local population.
However, further research is needed to quantify the potential efficiency gains of scaling up this model across the city.
The clinic has recently introduced an emergency respiratory service, which has already treated over 670 patients since its launch in December.
One patient, 77-year-old Christopher Thomas, who has chronic obstructive pulmonary disease, has benefited from the service, which allowed him to receive care at home rather than in hospital.
Thomas reports that the clinic's support enabled him to rest and manage his condition more effectively, with the added reassurance of being able to contact the team if concerns arose.
Respiratory medicine consultant Dr. Rifat Rashid praises the clinic's ability to provide rapid assessment and treatment, reducing delays and improving patient outcomes.
The clinic's impact extends to the hospital, where GPs are now referring patients directly to the clinic, and ambulances are bringing patients to the centre instead of the hospital.

Although the clinic has reduced admissions, the hospital remains full, as patients from other areas fill the available beds.
Plans are underway to expand the model across Birmingham, with the aim of establishing a network of six community hubs and 25-30 integrated neighbourhood teams to cover the city's population of 1.4 million.
Each hub will be tailored to meet the specific needs of its local population, with some focusing on supporting older adults with frailty.
The estimated costs of establishing the hubs are relatively low, at less than £100,000, as they will utilize existing buildings and redeployed staff.
Richard Kirby believes that the model could be easily replicated nationwide, but emphasizes that its success relies on the entire healthcare system embracing the approach.
He stressed that the model's effectiveness is contingent upon the willingness of all stakeholders to work together and adopt a more integrated, community-focused approach to care.
Ultimately, the success of this model will depend on its ability to be scaled up and replicated, while maintaining its core principles of collaboration, community engagement, and patient-centered care.
Financial constraints pose a significant obstacle to implementing a unified system, according to Ruth Rankine, primary care director at the NHS Confederation. During periods of fiscal austerity, collaboration among healthcare providers becomes increasingly challenging.
Rankine notes that when resources are scarce, healthcare providers tend to prioritize their immediate needs over collaborative efforts, focusing on allocating their limited budgets effectively.
However, clinics like Washwood Heath rely on cooperation and resource sharing to operate effectively, highlighting the need for a more integrated approach to healthcare.
Rankine also suggests that the hospital sector's skepticism has hindered progress in some areas. She emphasizes that investing in new initiatives can take time to yield results, often requiring years of commitment before tangible impacts are seen.
Another challenge lies in finding suitable facilities for healthcare services. Birmingham officials have acknowledged their fortunate position in having a network of large health centers, established through a short-lived finance program in the 2000s, but many other areas lack such infrastructure.
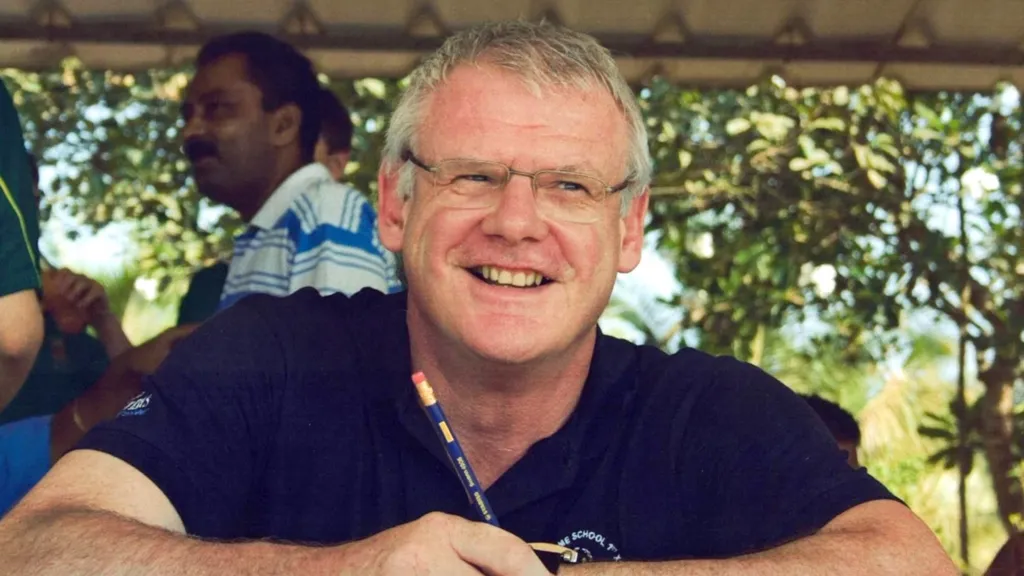
Dr. Richard Vautrey, a Leeds-based GP and former British Medical Association negotiator, has been involved in national NHS politics since the early 2000s and currently serves as president of the Royal College of GPs.
Vautrey argues that the lack of adequate premises is a significant concern, as many healthcare providers are forced to work in outdated and cramped facilities, making it difficult for GPs and community colleagues to collaborate effectively.
He questions the prioritization of resources, asking why there is a focus on building new hospitals rather than investing in neighborhood clinics, which he believes are essential for community-based care.
Deeper-seated political pressures also pose a challenge to implementing a nationwide network of community healthcare centers like those in Birmingham.
Despite the progress made in east Birmingham, which aligns with the recommendations outlined by Lord Darzi in his report to the government, commissioned by Wes Streeting, this is not the first time such initiatives have been proposed. Lord Darzi previously presented similar goals in a report to the Blair government in 2007.
Rankine, who worked at the Department of Health and NHS executive for over a decade from the mid-1990s, has witnessed these efforts firsthand. She notes that discussions about reforming the healthcare system have been ongoing for 20 to 30 years, yet significant progress has not been made.
The NHS currently faces a range of competing priorities, with the most pressing issues often taking precedence.
Hugh Alderwick, Director of Policy at the Health Foundation think-tank, observes that the current focus on meeting 18-week hospital waiting time targets may be at odds with the goal of shifting care to community-based services.
This contradiction in priorities can hinder efforts to reform the healthcare system and achieve the desired outcomes.
Dr. Vautrey remains optimistic about the potential for the government to transform the NHS into a neighborhood health service.
However, he emphasizes that achieving this goal will require determination, effort, and significant investment.
(No text provided, as this appears to be a credits section)
(No text provided, as this appears to be a promotional section)
(No text provided, as this appears to be a promotional section)
Health
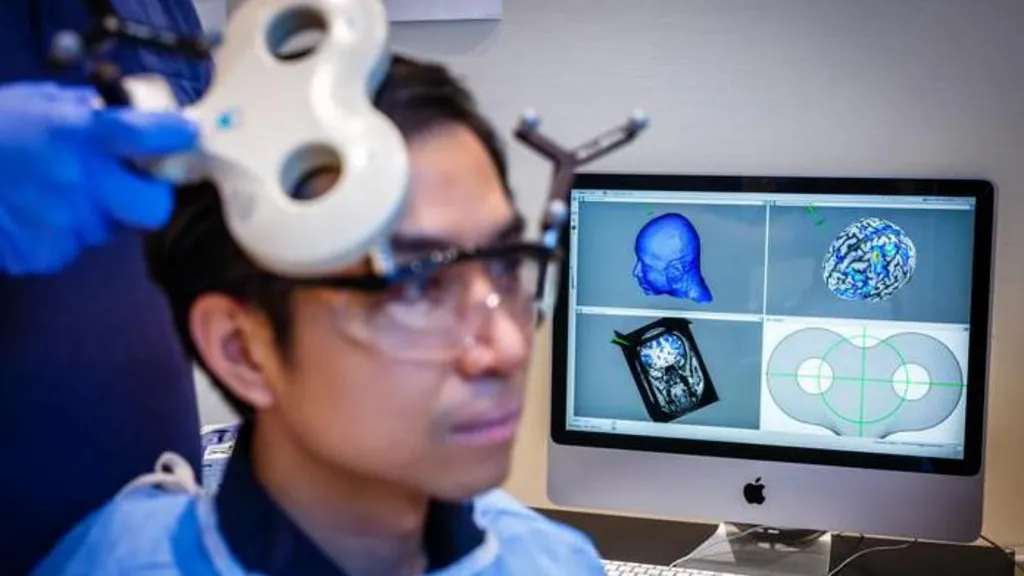
Study Explores if Brain Stimulation Can Reduce Selfish Behavior
Researchers have found a way to temporarily and marginally decrease self-centered behavior in individuals by activating two specific regions of the brain.
Researchers have made a groundbreaking discovery, finding that temporary reductions in selfish behavior can be achieved by stimulating specific areas of the brain.
A recent study conducted at the University of Zurich involved 44 participants who were tasked with dividing a sum of money between themselves and an anonymous partner, allowing scientists to observe their decision-making processes.
The experiment utilized electrical current to stimulate the frontal and parietal regions of the brain, located at the front and rear of the skull, respectively. When these areas were stimulated simultaneously, participants exhibited a greater willingness to share their funds.
According to Prof Christian Ruff, a lead author of the study, the observed effects were consistent, albeit modest in scale.
Statistical analysis revealed a notable increase in participants' willingness to allocate funds to others, indicating a shift in their behavior.
The findings not only provide insight into the neural mechanisms underlying fundamental human behavior but may also have implications for the treatment of certain brain disorders characterized by impaired social behavior.
Prof Ruff noted that some individuals struggle with profound social difficulties due to an inability to consider others' perspectives, leading to consistently selfish behavior, and suggested that this discovery could potentially be used to address such issues.
However, the effects of the brain stimulation were found to be short-lived, suggesting that repeated application may be necessary to achieve lasting changes.
Prof Ruff likened the potential effects of repeated stimulation to the benefits of regular exercise, stating that consistent application over a prolonged period could lead to significant changes in behavior, much like the physical adaptations that occur with regular gym attendance.
This latest discovery builds upon a previous study in which researchers monitored brain activity while participants engaged in a similar money-sharing game, providing a foundation for the current findings.
The earlier study identified two brain regions that appeared to be synchronized, with neural activity occurring at the same frequency, when participants made more generous decisions.
These brain areas are known to play a crucial role in decision-making and empathy, enabling individuals to distinguish between their own feelings and those of others.
When participants made selfless decisions, the regions responsible for empathy and decision-making were found to be communicating with each other.
The researchers sought to investigate whether electrical stimulation could be used to influence this communication and promote more selfless decision-making.
One participant who underwent the brain stimulation test described the experience as a gentle, soothing sensation, comparable to a warm shower or light rain on the scalp.
The participant reported making decisions while receiving the stimulation without feeling any external influence on their choices.
The discovery of a consistent neural pattern associated with selfless decision-making across multiple individuals suggests that altruism may be an innate, evolutionarily conserved trait that enables humans to care for one another.
Prof Ruff emphasized the clinical significance of this finding, highlighting the potential to modify and influence this neural mechanism.
Dr Jie Hu, a co-author of the study, noted that the research provides evidence of a causal relationship between brain activity and decision-making, demonstrating that targeted stimulation can alter an individual's sharing behavior.
By manipulating communication within a specific brain network using non-invasive stimulation, the researchers observed a shift in participants' decisions, influencing the balance between self-interest and altruism.
Addressing concerns about the potential implications of this research, Prof Ruff assured that the experiment was conducted with strict adherence to medical regulations and ethical guidelines, ensuring the well-being and informed consent of all participants.
The neuroscientist drew a distinction between the controlled, medically regulated nature of the experiment and the often-subliminal influences of social media and advertising, which can affect behavior without explicit consent.
Prof Ruff suggested that, in contrast to the experiment, the impacts of social media and advertising on brain function and behavior are often unforeseen and uncontrolled, highlighting the importance of careful consideration and regulation in such contexts.
Health
NHS Workers to Receive 3.3% Pay Increase
Labor unions have expressed displeasure, yet the government maintains that its actions showcase a dedication to its workforce.
The government has confirmed that NHS staff in England will receive a 3.3% pay increase in the upcoming financial year.

This pay award applies to approximately 1.4 million health workers, including nurses, midwives, physiotherapists, and porters, but excludes doctors, dentists, and senior management.
Although the Department of Health and Social Care initially proposed a lower figure, it has accepted the recommendation of the independent pay review body to demonstrate its commitment to NHS staff, resulting in a higher pay rise than initially suggested.
However, several health unions have expressed disappointment with the announced pay award.
Prof Nicola Ranger, general secretary of the Royal College of Nursing (RCN), noted that the 3.3% increase falls short of the current consumer price index (CPI) inflation rate of 3.4%, which measures the rise in prices over the past year.
Prof Ranger stated, "A pay award that is lower than the current inflation rate is unacceptable, and unless inflation decreases, the government will be imposing a real pay cut on NHS workers."
She criticized the government's approach, saying, "This strategy of making last-minute decisions is not an appropriate way to treat individuals who are essential to a system in crisis."
Prof Ranger indicated that she would wait to see the pay awards for the rest of the public sector and doctors before deciding on a course of action.
The RCN had previously reacted strongly to the 5.4% pay increase received by resident doctors last year, compared to the 3.6% increase received by nurses, which they described as "grotesque".
Prof Ranger emphasized, "Nursing staff will not accept being treated with disrespect, as has happened in the past when they were given lower pay awards than other groups."
Helga Pile, head of health at Unison, the largest health union, commented, "NHS staff who are already under financial pressure will be outraged by another pay award that fails to keep up with inflation."
"Once again, they are expected to deliver more while their pay effectively decreases, as it falls behind the rising cost of living," she added.
In response, the government argued that the pay award is actually above the forecasted inflation rate for the coming year, which is around 2%.
A spokesperson for the Department of Health and Social Care stated, "This government greatly values the outstanding work of NHS staff and is committed to supporting them."
The pay increase is expected to be implemented by the start of April.
However, the government did not provide a timeline for the announcement on doctors' pay, as the pay review body responsible for making recommendations on their pay has yet to submit its report to ministers.
The government is currently engaged in negotiations with the British Medical Association regarding the pay of resident doctors, previously known as junior doctors.
Members of the BMA recently voted in favor of strike action, granting them a six-month mandate for walkouts, and there have been 14 strikes so far in the ongoing dispute.
Health
NHS Waiting List Hits Three-Year Low
In England, the backlog has fallen below 7.3 million for the first time since 2023, yet worries persist regarding prolonged waiting times in accident and emergency departments.
England's hospital waiting list has reached its lowest point in almost three years, marking a significant milestone in the country's healthcare system.

As of December 2025, the number of patients awaiting treatment, including knee and hip operations, stood at 7.29 million, the lowest figure recorded since February 2023.
However, the latest monthly update from NHS England reveals that long wait times persist in Accident and Emergency departments, with a record number of patients experiencing 12-hour trolley waits.
In January 2026, over 71,500 patients spent more than 12 hours waiting for a hospital bed after being assessed by A&E staff, the highest number tracked since 2010.
This translates to nearly one in five patients admitted after visiting A&E waiting for an extended period.
According to Health Secretary Wes Streeting, while progress has been made, significant challenges still need to be addressed.
Streeting acknowledged that "there is much more to do" and emphasized the need to accelerate progress, but expressed optimism that the NHS is on the path to recovery.
Dr. Vicky Price, representing the Society for Acute Medicine, noted that hospitals are operating beyond safe capacity in terms of emergency care.
Dr. Price highlighted the vulnerability of patients who require admission, often elderly and frail individuals with complex needs, who are at greater risk of harm when care is delivered in corridors and hospitals exceed safe limits.
Duncan Burton, Chief Nursing Officer for England, commended the progress made in reducing wait times, achieved despite the challenges posed by strikes by resident doctors.
Burton attributed this progress to the hard work and dedication of NHS staff, describing it as a "triumph".
Although the waiting list decreased, performance against the 18-week target slightly declined, with 61.5% of patients waiting less than 18 weeks, compared to 61.8% in November, and still short of the 92% target set to be met by 2029.
Rory Deighton of the NHS Confederation, which represents hospitals, welcomed the progress but cautioned that it obscures significant regional variations.
A recent BBC report revealed that nearly a quarter of hospital trusts experienced worsening wait times over the past year.
Deighton emphasized that the NHS is composed of numerous separate organizations, each with unique financial and operational challenges, making it more difficult to address care backlogs in some areas.
According to Deighton, this means that tackling care backlogs will be more challenging in certain parts of the country due to these distinct regional challenges.
-

 News8 hours ago
News8 hours agoAustralian Politics Faces Questions Over Gender Equality Amid Sussan Ley’s Appointment
-
 News5 hours ago
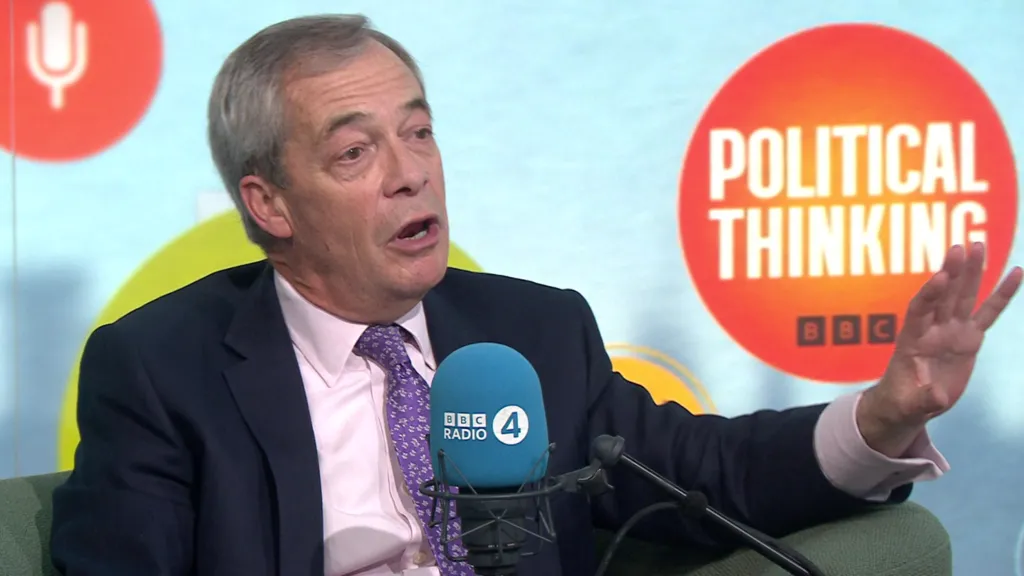
News5 hours agoFarage Says Reform to Replace Traditional Tory Party
-

 News5 hours ago
News5 hours agoWrexham Pair Seek Win Against Former Team Ipswich
-

 News11 hours ago
News11 hours agoLiberal Party Removes Australia’s First Female Leader
-

 News9 hours ago
News9 hours agoUK Braces for Cold Snap with Snow and Ice Alerts Expected
-
 News5 hours ago
News5 hours agoHusband’s alleged £600k theft for sex and antiques blamed on drug side effects
-

 News2 days ago
News2 days agoSunbed ads spreading harmful misinformation to young people
-

 Business11 hours ago
Business11 hours agoBBC Reporter Exposed to Cyber Attack Due to Vulnerabilities in AI Coding Tool